12 Action Steps
STEP 3: Take your QAPI “Pulse” with a Self-Assessment
In order to establish QAPI in your organization, it is helpful to conduct a self-assessment in your organization. As you continue implementing the action steps outlined in this guide, you should periodically evaluate QAPI in your organization – see how far you’ve come.
To get you started, we’ve developed a self-assessment tool to take your QAPI “pulse.” It will assist you in evaluating the extent to which components of QAPI are in place within your organization and identifying areas requiring further development. It will help you determine how you really know whether QAPI is taking hold.
You may use the self-assessment tool as you begin work on QAPI and then for annual or semiannual evaluation of your organization’s progress. You should complete the tool with input from the entire QAPI team and organizational leadership. This is meant to be an honest reflection of your progress with QAPI. The results of this assessment will direct you to areas you need to work on in order to establish QAPI in your organization.
https://www.cms.gov/medicare/provider-enrollment-and-certification/qapi/downloads/qapiataglance.pdf
QAPI Self-Assessment Tool

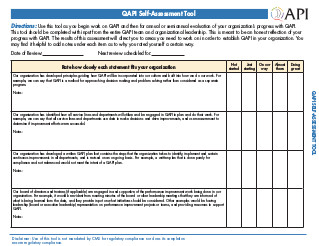
Directions: Use this tool as you begin work on QAPI and then for annual or semiannual evaluation of your organization’s progress with QAPI. This tool should be completed with input from the entire QAPI team and organizational leadership. This is meant to be an honest reflection of your progress with QAPI. The results of this assessment will direct you to areas you need to work on in order to establish QAPI in your organization. You may find it helpful to add notes under each item as to why you rated yourself a certain way.
Date of Review:_____________ Next review scheduled for:_____________
| Rate how closely each statement ts your organization | Not started | Just starting | On our way | Almost there | Doing great |
|---|---|---|---|---|---|
|
Our organization has developed principles guiding how QAPI will be incorporated into our culture and built into how we do our work. For example, we can say that QAPI is a method for approaching decision making and problem solving rather than considered as a separate program. Notes: |
|||||
|
Our organization has identi ed how all service lines and departments will utilize and be engaged in QAPI to plan and do their work. For example, we can say that all service lines and departments use data to make decisions and drive improvements, and use measurement to determine if improvement efforts were successful. Notes: |
|||||
|
Our organization has developed a written QAPI plan that contains the steps that the organization takes to identify, implement and sustain continuous improvements in all departments; and is revised on an ongoing basis. For example, a written plan that is done purely for compliance and not referenced would not meet the intent of a QAPI plan. Notes: |
|||||
|
Our board of directors and trustees (if applicable) are engaged in and supportive of the performance improvement work being done in our organization. For example, it would be evident from meeting minutes of the board or other leadership meetings that they are informed of what is being learned from the data, and they provide input on what initiatives should be considered. Other examples would be having leadership (board or executive leadership) representation on performance improvement projects or teams, and providing resources to support QAPI. Notes: |
|||||
|
QAPI is considered a priority in our organization. For example, there is a process for covering caregivers who are asked to spend time on improvement teams. Notes: |
|||||
|
QAPI is an integral component of new caregiver orientation and training. For example, new caregivers understand and can describe their role in identifying opportunities for improvement. Another example is that new caregivers expect that they will be active participants on improvement teams. Notes: |
|||||
|
Training is available to all caregivers on performance improvement strategies and tools. Notes: |
|||||
|
When conducting performance improvement projects, we make a small change and measure the effect of that change before implementing more broadly. An example of a small change is pilot testing and measuring with one nurse, one resident, on one day, or one unit, and then expanding the testing based on the results. Notes: |
|||||
|
When addressing performance improvement opportunities, our organization focuses on making changes to systems and processes rather than focusing on addressing individual behaviors. For example, we avoid assuming that education or training of an individual is the problem, instead, we focus on what was going on at the time that allowed a problem to occur and look for opportunities to change the process in order to minimize the chance of the problem recurring. Notes: |
|||||
|
Our organization has established a culture in which caregivers are held accountable for their performance, but not punished for errors and do not fear retaliation for reporting quality concerns. For example, we have a process in place to distinguish between unintentional errors and intentional reckless behavior and only the latter is addressed through disciplinary actions. Notes: |
|||||
|
Leadership can clearly describe, to someone unfamiliar with the organization, our approach to QAPI and give accurate and up-to-date examples of how the facility is using QAPI to improve quality and safety of resident care. For example, the administrator can clearly describe the current performance improvement initiatives, or projects, and how the work is guided by caregivers involved in the topic as well as input from residents and families. Notes: |
|||||
|
Our organization has identi ed all of our sources of data and information relevant to our organization to use for QAPI. This includes data that re ects measures of clinical care; input from caregivers, residents, families, and stakeholders, and other data that re ects the services provided by our organization. For example, we have listed all available measures, indicators or sources of data and carefully selected those that are relevant to our organization that we will use for decision making. Likewise, we have excluded measures that are not currently relevant and that we are not actively using in our decision making process. Notes: |
|||||
|
For the relevant sources of data we identify, our organization sets targets or goals for desired performance, as well as thresholds for minimum performance. For example, our goal for resident ratings for recommending our facility to family and friends is 100% and our threshold is 85% (meaning we will revise the strategy we are using to reach our goal if we fall below this level). Notes: |
|||||
|
We have a system to effectively collect, analyze, and display our data to identify opportunities for our organization to make improvements. This includes comparing the results of the data to benchmarks or to our internal performance targets or goals. For example, performance improvement projects or initiatives are selected based on facility performance as compared to national benchmarks, identi ed best practice, or applicable clinical guidelines. Notes: |
|||||
|
Our organization has, or supports the development of, employees who have skill in analyzing and interpreting data to assess our performance and support our improvement initiatives. For example, our organization provides opportunities for training and education on data collection and measurement methodology to caregivers involved in QAPI. Notes: |
|||||
|
From our identi ed opportunities for improvement, we have a systematic and objective way to prioritize the opportunities in order to determine what we will work on. This process takes into consideration input from multiple disciplines, residents and families. This process identi es problems that pose a high risk to residents or caregivers, is frequent in nature, or otherwise impact the safety and quality of life of the residents. Notes: |
|||||
|
When a performance improvement opportunity is identi ed as a priority, we have a process in place to charter a project. This charter describes the scope and objectives of the project so the team working on it has a clear understanding of what they are being asked to accomplish. Notes: |
|||||
|
For our Performance Improvement Projects, we have a process in place for documenting what we have done, including highlights, progress, and lessons learned. For example, we have project documentation templates that are consistently used and led electronically in a standardized fashion for future reference. Notes: |
|||||
|
For every Performance Improvement Project, we use measurement to determine if changes to systems and process have been effective. We utilize both process measures and outcome measures to assess impact on resident care and quality of life. For example, if making a change, we measure whether the change has actually occurred and also whether it has had the desired impact on the residents. Notes: |
|||||
|
Our organization uses a structured process for identifying underlying causes of problems, such as Root Cause Analysis. Notes: |
|||||
|
When using Root Cause Analysis to investigate an event or problem, our organization identi es system and process breakdowns and avoids focus on individual performance. For example, if an error occurs, we focus on the process and look for what allowed the error to occur in order to prevent the same situation from happening with another caregiver and another resident. Notes: |
|||||
|
When systems and process breakdowns have been identi ed, we consistently link corrective actions with the system and process breakdown, rather than having our default action focus on training education, or asking caregivers to be more careful, or remember a step. We look for ways to assure that change can be sustained. For example, if a policy or procedure was not followed due to distraction or lack of caregivers, the corrective action focuses on eliminating distraction or making changes to staffing levels. Notes: |
|||||
|
When corrective actions have been identi ed, our organization puts both process and outcome measures in place in order to determine if the change is happening as expected and that the change has resulted in the desired impact to resident care. For example, when making a change to care practices around fall prevention there is a measure looking at whether the change is being carried out and a measure looking at the impact on fall rate. Notes: |
|||||
|
When an intervention has been put in place and determined to be successful, our organization measures whether the change has been sustained. For example, if a change is made to the process of medication administration, there is a plan to measure both whether the change is in place, and having the desired impact (this is commonly done at 6 or 12 months). Notes: |